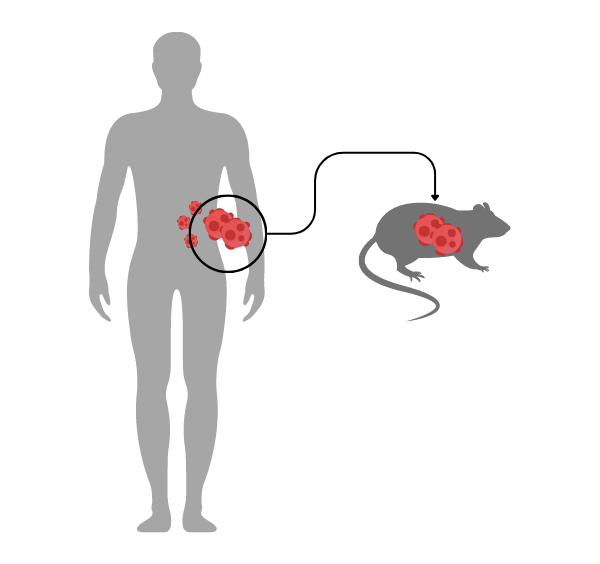
PDX models are a critical type of preclinical model used in cancer research. In PDX models, cancerous tumor tissue from a human patient is implanted into immunodeficient mice or other host animals. The implanted tumor is then allowed to grow in the host, providing researchers with a model system to study tumor growth, metastasis, and response to potential therapies.
The Fundamentals of PDX Models
Tissue Collection and Preparation
Viable tumor tissue is obtained through surgery or biopsy and then processed into small fragments — though, they must be of sufficient size to improve the chances of successful engraftment in the host. Depending on the specific PDX model, the tissue may be implanted directly or combined with extracellular matrix components to facilitate engraftment.
Implantation
The prepared tumor tissue is implanted into the host animal, typically by surgical means. The implantation site can vary depending on the cancer type being studied. Subcutaneous implantation is common, but orthotopic implantation (implanting the tumor in the same organ as the original tumor) can provide a more relevant microenvironment for tumor growth.
Tumor Monitoring
The implanted tissue is monitored for growth in the host animal. This may involve periodic measurements of tumor size with imaging techniques or other methods. It can take several months for a tumor to establish and grow to a sufficient size for further study.
Experimental Intervention and Analysis
Once the tumor is established, testing of potential therapies or interventions commences. This may involve administering drugs, radiation therapy, or other treatments to the host animal, followed by monitoring tumor response. After the intervention, the tumor tissue can be collected, analyzed, and compared with pre-treatment samples to assess the effectiveness of the treatment.
Comparing PDX to Cell Line-derived Xenograft (CDX) Models
CDX models use established cancer cell lines that have been grown and maintained in vitro, whereas PDX models use fresh tumor tissue obtained directly from human patients. As a result, PDX models better preserve the original tumor's cellular heterogeneity and architecture, which can be important for accurately studying tumor biology and response to treatments. CDX models, on the other hand, often lose some of this heterogeneity due to the adaptation of cells to in vitro culture conditions.
CDX models, however, are generally easier and faster to establish and maintain because cancer cell lines can be quickly grown in vitro and cryopreserved for future use; PDX models, by contrast, require the continuous engraftment of fresh patient-derived tumor tissue. CDX models are also often more consistent and reproducible, as cell lines can be easily standardized and shared between research groups. PDX models have more variability due to differences in patient-derived tumors and engraftment success rates.
The Advantages of PDX Models
Tumor Heterogeneity
PDX models preserve the original tumor's cellular heterogeneity, architecture, and complexity, providing a more accurate representation of human tumors than traditional cancer cell lines or CDX models.
Tumor Microenvironment
Because they maintain elements of the patient's tumor microenvironment, PDX models allow for a more relevant study of tumor biology and treatment response.
Personalized Medicine
PDX models facilitate personalized treatment strategies for individual patients based on the response of their tumor tissue in the model system.
Predictive Value
Models like PDX that closely mimic the biology and behavior of human tumors have been shown to better predict patient response to therapies.
Insight into Rare Tumor Types and Genetic Mutations
PDX models can be generated for rare tumor subtypes or tumors with specific genetic mutations, which may not be well-represented in existing cancer cell lines.
The Disadvantages of PDX Models
Immunodeficient Hosts
Immunodeficient host animals, a necessity for PDX, limit the study of the immune system's role in cancer progression and response to immunotherapies.
Establishment and Maintenance
PDX models have varying success rates for engraftment and growth depending on the tumor type. Additionally, they can be more time-consuming and resource-intensive compared to other models.
Tumor Adaptation
Over time, the tumor tissue in a PDX model may adapt to the host animal's environment, which could result in changes in tumor behavior or treatment response that may not be representative of the original patient's tumor.
Host Microenvironment
Although PDX models maintain some elements of the human tumor microenvironment, the host animal's microenvironment can still influence tumor behavior, which may not accurately reflect the tumor's behavior in a human patient.
Bioethical Considerations
The use of animals, particularly immunodeficient mice, for PDX models raises concerns regarding animal welfare.
Scalability
Because PDX models rely on patient-derived tumor samples, which can vary in availability and quality, standardizing a large study brings added challenges.
Advanced PDX Capabilities
There are numerous methodologies, many of which are still emerging, that can enhance the efficiency and effectiveness of a PDX model, such as complementary 2D and 3D in vitro assays and in vivo services that provide additional information about tumor biology, response to treatments, and mechanisms of action. These tools can help overcome some of the limitations of PDX models and provide a more comprehensive understanding of cancer.
Other enhancements to a PDX model can include subcutaneous, orthotopic, and disseminated models; molecular and pharmacological characterization (e.g. genomic, transcriptomic, and proteomic analyses); an integrated approach that combines PDX models with their corresponding cell lines; and the identification of biomarkers predicting tumor sensitivity, which can help guide drug development and personalize treatment strategies.
While the use of complementary assays and in vivo services can enhance PDX models, as with all clinical research, deep scientific expertise is foundational for optimizing model establishment and maintenance, accurately interpreting results, integrating complementary approaches, and translating findings to clinical research.
LIDE delivers innovations in oncology translational research and immuno-oncology. Contact us today to learn more about our first-class research capabilities.
LIDE delivers innovations in oncology translational research and immuno-oncology. Contact Global Vice President, Josh Caggiula today to learn more about our first-class research capabilities.