A xenograft is a clinical or research procedure where soft tissue or organ material is transplanted from one species into a different species. In clinical medicine, xenografts have been used in certain cases where human tissue or organs are not readily available for transplantation. Xenografts can also be used in medical research to study the function and behavior of various tissues and organs, as well as to develop new treatments and therapies for diseases.
Clinical Uses
One of the primary applications of xenografts is tissue engineering. Xenografts can be used to create tissues and organs for transplantation. By transplanting animal tissue into a human recipient, researchers can develop new methods for growing human tissue or repairing organ damage, such as in the case of xenograft bioprosthetic heart valves derived from pigs.
There are only a small number of animal species that have been approved for use in xenografts, but the number of commercially available products based on this science is growing rapidly. The most common xenograft product on the market today is EZ Derm®, and an aldehyde cross-linked porcine dermis (pig skin that has been chemically treated to make it safe for use in human surgeries). Clinical use of xenografts is now relatively common for a wide variety of soft tissue augmentation procedures, including:
- Dural Repair
- Chest Wall Reconstruction
- Cardiac and Cardiovascular Surgery
- Abdominal Wall Repair
- Pelvic Organ Prolapse Repair
Autografts, Allografts, and Xenografts
The treatment of skin damaged by burns is one of the most common applications of surgical grafting. The preference of medical professionals in those cases is to use human-derived skin grafts, which greatly reduces the risk of rejection. Grafts taken from the patient’s own body, referred to as autografts, are naturally the option with the lowest risk of rejection. If that is not feasible, living donor tissue from a genetically similar individual may be used. If living donor tissue is not available in any form, cadaver-derived grafts, called allografts, are considered.
Another method of extending a limited supply of donor tissue is a mesh graft, where the skin is stretched and sliced into a mesh. This method naturally extends the size of the graft but adds complexity to the procedure and requires a longer recovery period.
However, in severe cases, there may be insufficient human tissue to cover the damaged areas. To make up for that shortfall, tissue from another species may be temporarily grafted onto the wound. The foreign material acts like a scaffold, allowing the patient's own cells to grow and rebuild the missing tissue. Xenograft products are an especially effective tool to combat partial-thickness skin loss and will protect exposed tissues from external contaminants while significantly slowing the advent of protein loss and cell death.
The Drawbacks of Xenografts
Because the genetic differences between the donor and recipient are greater in a xenograft, the risk of rejection by the recipient's immune system is much higher than in an autograft or allograft. Additionally, there is a risk of transmission of diseases from the donor species to the recipient.
Furthermore, xenografts are not typically considered a permanent solution because of the risk of rejection and other complications. A xenograft may be able to function effectively for a period of time, but the risk of rejection by the recipient's immune system is high, which can lead to graft failure over time. In most cases, a xenograft is a stopgap solution. Once more suitable donor tissue is available or the damaged tissue has healed to an acceptable state, it is typically removed.
Research Applications
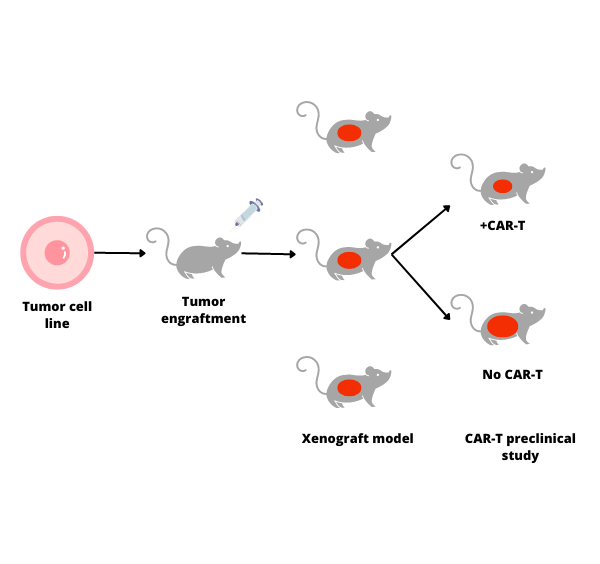
In addition to clinical procedures, xenografts are a vital tool in several areas of medical research, notably oncology and drug therapy studies. Patient-Derived Xenografts (PDX) involve the transplantation of a human’s tissue, such a segment of a tumor, into an immunodeficient or humanized mouse. The goal of the research is to analyze the growth patterns and behavior of the tumor and develop personalized treatment protocols.
The PDX can be transplanted under the skin or directly into the same organ in the foreign species from which it originally developed in the human. There is a significant body of research in rodent PDX models, and immunodeficient or humanized animal test subjects are used to reduce the risk of rejection of foreign tissue. Once implanted in the test animal, cancer drugs or other treatment modalities are trialed on the PDX to study their safety and efficacy before attempting to use them on the human patient.
The Ethics of Xenografts
Despite their proven effectiveness and the potential for future advancements in the field of xenografts, there are non-trivial bioethics concerns surrounding them. Xenotransplantation animals must be kept under strictly controlled laboratory conditions, which prevents them from developing infections, diseases, or parasites that could be transmitted to the recipient of their tissue. Such conditions exist to ensure human safety but at the expense of the animal’s own welfare.
Ultimately, the use of xenografts must be balanced against ethical considerations related to animal welfare and human health, and must be subject to appropriate ethical and regulatory oversight.
LIDE delivers innovations in oncology translational research and immuno-oncology. Contact Global Vice President, Josh Caggiula today to learn more about our first-class research capabilities.